Vyne Dental is committed to helping you improve your dental practice’s revenue cycle with its comprehensive set of solutions to streamline eligibility, expedite reimbursements, and improve communication with your patients and your team.
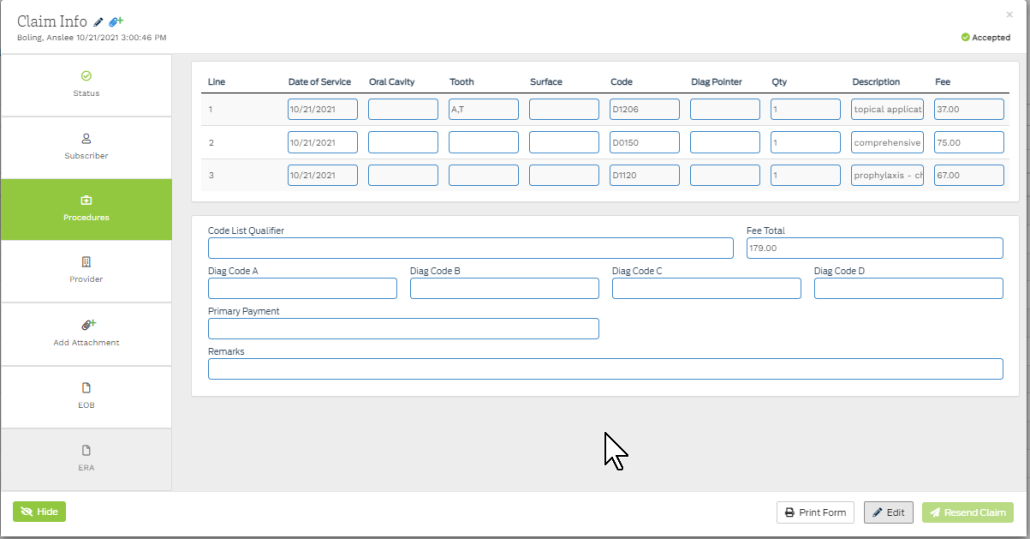
The Vyne Trellis™ platform is an end-to-end dental billing solution that provides dental claims management, including simple, integrated electronic attachments, batch and real-time eligibility and benefits, with connections to hundreds of insurance payers, all in one intuitive, easy-to-use solution.
A few of Vyne Trellis’ most innovative features include:
- Batch and Real-time benefit plan eligibility verification to reduce the time practice team members spend on the phone with payers — office managers and billers receive verification of patient benefits within seconds through the Vyne Trellis web-based platform;
- A robust electronic attachment submission solution , that’s connected to more than 800 payers across the country;
- A feature-rich portal that integrates a practice’s submitted, processed, and paid claims, supporting attachments and documentation, and eligibility status — to each patient and their respective payer; and
- Intelligent validation engine to identify potential errors, such as missing subscriber IDs, claim form information, attachment requirements, and patient and provider detail, before electronically submitting claims to a payer — reducing rejected claims, creating efficiency in the billing workflow, and accelerating reimbursements back into the practice.
Vyne Trellis continues to evolve
Vyne Trellis continues to evolve and, in so doing, redefine what “revenue cycle management solution” means to the dental practice. Earlier this year Vyne Dental strategically expanded its portfolio to add simple, customizable electronic forms, text and email reminders, on-line reviews, and secure communications, including email and inter-office chat. This strategic shift allows dental practices on Vyne Trellis to initiate the electronic, automated interaction with their patients much earlier in their journey, thus ensuring a timely resolution to all revenue collection attempts, while simultaneously improving patient experience, reducing friction, and cutting costs.
Vyne Trellis eligibility and benefits verification
The Vyne Trellis real-time and batch eligibility feature helps any dental practice reduce the amount of time spent on manual interactions with payers. The instant claims validation system also identifies potential errors on submitted claims, like a missing insurance subscriber number, before submitting documents to your payers.
Thanks to this intelligent feature, you’ll reduce your practice’s rejected claims, as well as speed up adjudication and drive revenue for the practice.
Verifying eligibility is tedious and time-consuming, but it’s a crucial step toward ensuring your practice’s financial success and enriching patient relationships, and Vyne Trellis makes it more manageable!
Vyne Trellis automated eligibility
In most major Practice Management Systems, Vyne Trellis can see subscriber details, the patients’ carrier, provider, and appointment information and send an eligibility request automatically, eliminating your need to check manually. This saves your team time by reducing the manual entry of patient details to send a request to payers before a scheduled appointment date.
Furthermore, automated eligibility verifies eligibility for patients with a scheduled appointment in your supported practice management software three days before a scheduled appointment. It enables staff to view responses without manually sending a request.
The new eligibility design offers easy searching and filtering by rows. This feature is currently available for Open Dental customers, with Dentrix and EagleSoft integrations coming shortly. This feature alone is one of the most well-understood and frequently endured pain points in any dental practice. Vyne Trellis helps eliminate it!
Additional new Vyne Trellis features
In addition to Vyne Trellis helping streamline every aspect of your practice’s revenue cycle and automating your claims management, the solution now features several new, cutting-edge tools to help power your practice. Specifically, we’ve made the most common searches available in a single dashboard to shave minutes off of your workflows each day, but we’ve included many other important features:
- Electronic Patient Forms We’ve added our newly acquired OperaDDS solution features into the Vyne Dental(R) portfolio, including its secure communication and form creation capabilities. For example, forms and form creation are electronic and fully customizable – virtually any form of any kind can be created for any purpose.
- Text and Email Reminders In addition to the simple, yet powerful electronic forms, OperaDDS adds a robust reminder system with automated texts and emails to help ensure patients are confirmed for their appointments and show up on time!
- Secure email* Vyne Dental’s secure email solution is also built right in. So it’s the perfect and safe way for your practice to communicate sensitive and personal health information with specialist providers and patients.
- Patient Reviews With the integration of OperaDDS, Vyne Dental now allows your practice to manage its online reviews from patients. Positive reviews are automatically funneled to the review boards. Reviews from patients that rate below a certain threshold (negative reviews) are routed directly to the practice manager to address any potential issues.
- Intra-office chat Vyne Trellis now includes an intra-office chat feature that allows practice employees to communicate inside the practice quickly on a multitude of devices, including your smartwatch! Doctors can see when patients are ready, if there is an emergency in the waiting room, or even if lunch has arrived. Internal chat capabilities help remove workflow friction present in most dental practices today and is a proven productivity booster!
Built with feedback from real users
These latest features from Vyne Trellis result from our industry understanding, experience, and direct, real-time feedback from users. We maintain multiple feedback loops with users and are always on the hunt for insights and priorities as we continue to invest in our solutions.
Along with all of these high-impact developments, Vyne Dental continues to add more payer connections to support our eligibility responses and ensure electronic connectivity for all of your claims and attachments. As the number of connections grows, the better our solutions can serve the needs of your practices.
Vyne Dental currently has more than 800 connections to dental insurance payers and, as a result, we help your claims get paid more quickly and efficiently.
Ultimately, Vyne Dental is helping to alleviate pain in the dental practice revenue cycle management. Providing access to real-time eligibility, for example, keeps you better informed on patient plan maximums, deductibles, and their care utilization. In addition, it can verify whether some procedure codes are covered under a patient’s benefit plan – important to reducing the daily minutia.
Vyne Trellis is exceptionally user-friendly and allows billing managers to monitor claims from their dashboard, creating tremendous efficiency for the entire practice. At Vyne Dental, we aim to help you improve nearly every facet of your administrative demands so that you can continue to focus on patient care.
Connect with us to learn more!
We’d love to show you all of Vyne Trellis’ features and how they can help improve your revenue cycle and claims management processes! For additional information on Vyne Trellis, visit the solution page here!
(c)2021 Napa EA/MEDX LLC. All rights reserved. All third-party trademarks and tradenames (including logos and icons) referenced are and remain the property of their respective owners.
*Secure Email is email transmission functionality that requires login credentials for access, is encrypted at rest, allows for email delivery revocation, auto-expiration for access to data, recipient authentication and read receipts. Use of Secure Email does not guarantee additional or absolute security.