Secondary Claims – Adjustment Information: A Quick Update from the Solutions Team at Vyne Dental
Have you noticed a recent uptick in secondary claim rejections? You’re not alone, we’ve seen it too, and we’re here to help.
Here’s what we know so far.
There is a growing list of insurance carriers that are requiring that claim adjustment information be included on secondary claims. Additionally, the current ADA claim form does not provide a dedicated field for financial information related to secondary claims.
What does this mean for you?
If an insurance carrier now requires this adjustment information on all secondary claims, they may reject any secondary claim that’s missing it.
So what can you do about it today?
Vyne Dental can help support the successful submission of your secondary claims, to insurance carriers who require adjustment information, by submitting the required information in the ‘Remarks’ field on said claims.
Here’s how:
-
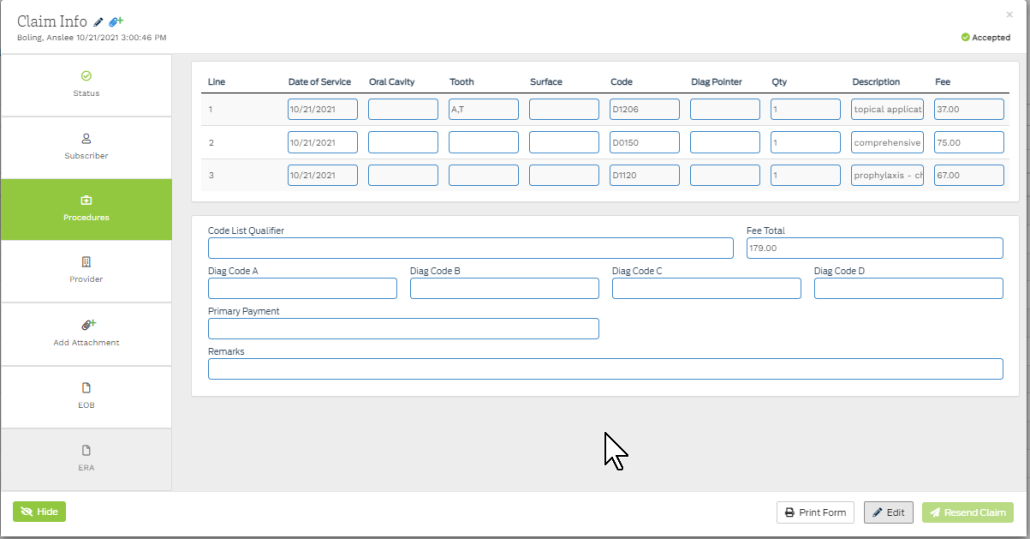
- Send the claim to the Queue and navigate to the Procedures Tab
- Enter the Primary Payment in the box provided; and enter the adjustment information in the remarks section: (see examples here)
- We’ll send the required information, electronically, on your behalf along with the rest of your claim data, to the insurance carrier.
Here’s a peek into our long-term strategy for a more permanent solution.
Vyne Trellis will detect that a secondary claim requires the adjustment information and automatically add it for you, reducing manual entry and error.