Discover Vyne
Intelligent Exchange
Leveraging state-of-the-art technology to redefine the way insurance payers prioritize and optimize clinical claim reviews by automating high touch manual claim processing workflows.
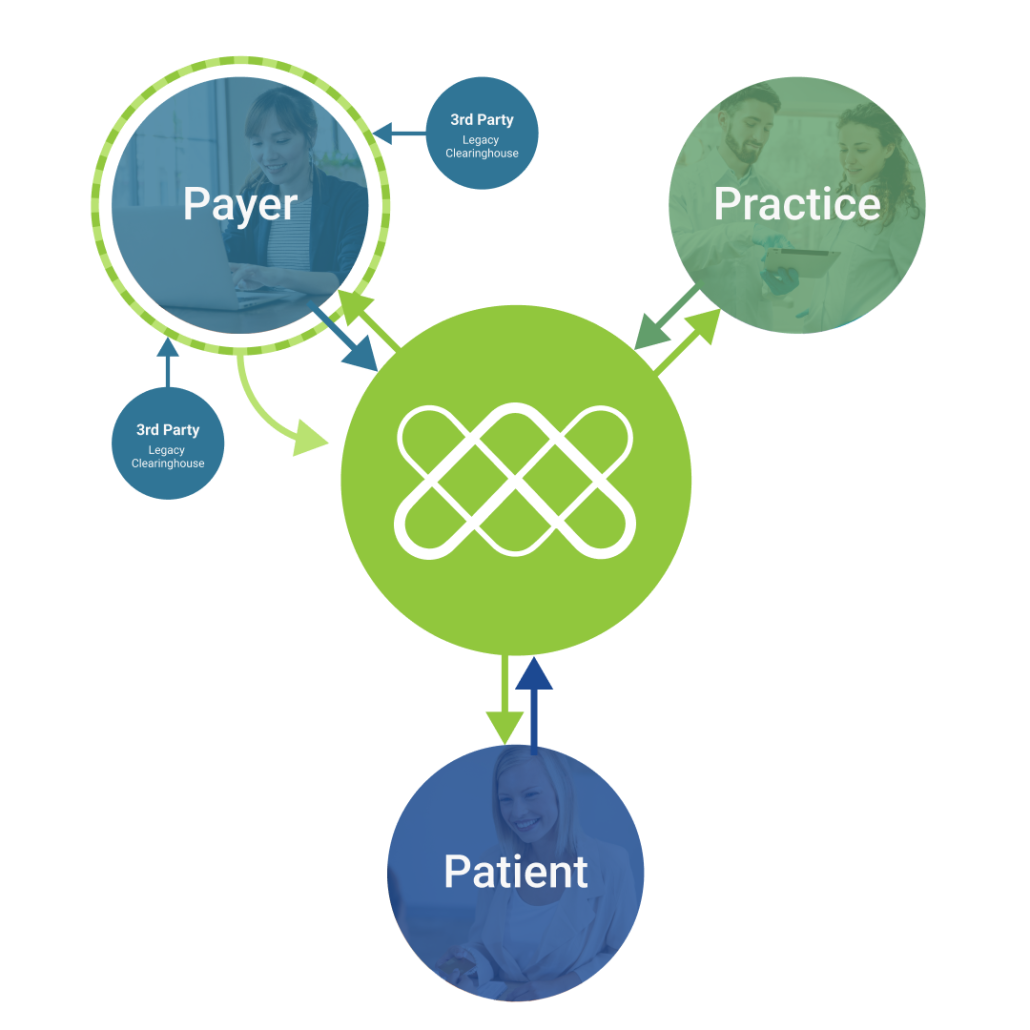
An Intelligent Choice Uniquely Positioned Between Provider and Payer
This integrated AI service offering to payers includes notifying provider’s staff of identified correctable errors, allowing the provider to remediate identified errors including:
Missing documentation
Undiagnosable image quality
Duplicate image detected
Incorrect patient
Incorrect dentition/ anatomy
Medical necessity evident

See how pairing our clearinghouse connectivity and proven AI helped to identify millions of dollars in savings for this dental payer.

What is Vyne Intelligent Exchange?
In strict adherence to the payer’s custom rules, Vyne Intelligent Exchange combines its traditional Electronic Data Interchange, its modern REST API, and Artificial Intelligence* powered by NovoDynamics to facilitate the delivery of a clean claim with all of the requisite, legible documentation, helping payers confidently increase auto-adjudication rates, decrease operating expenses, and optimize key cost centers like clinical review.
Benefits
Vyne Intelligent Exchange utilizes Intelligent clearinghouse level preprocessing to:
Reduce incidents of claims with insufficient documentation and requests for additional information
Proactively identify with each image the sufficient quality and appropriate anatomy, visible tooth numbers, and duplicate or altered images
Accurately and consistently identify claims that require review or down-coding
Confidently increase auto-adjudication rates
Reduce erroneously paid claims
Optimize clinical review staff with prioritized work queue based on AI confidence and potential savings

What does this mean?
For Providers
Vyne Intelligent Exchange empowers dental staff to preemptively remediate errors made during claim creation. Providers appreciate the upfront visibility and opportunity to eliminate potential claims processing delays.
For Payers
Vyne Intelligent Exchange claims will be delivered to payers with annotations indicating that the claim has been analyzed using AI and a recommendation to either:
- Approve the claim as billed or
- Flag and prioritize the claim as a potential denial that requires further clinical review
Ready to partner with Vyne Dental and revolutionize your approach for optimizing the clinical claim review process?
Submit the form below and we’ll connect with you.